Meet the People of the Irsay
Meet our directors, faculty leadership, scholars, staff, and advisory board members
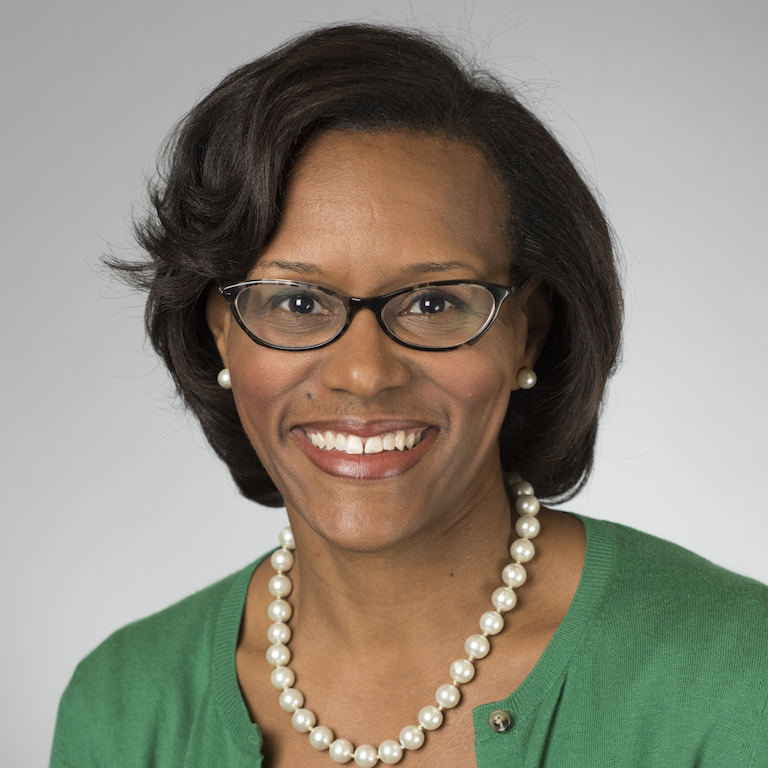
Brownsyne Tucker Edmonds
Continuity Lead
- Phone:
- (317) 944-1661
- Email:
- btuckere@iu.edu
- Campus:
- IUI
- Website:
- Visit website
Biography
Tucker-Edmond’s research targets three areas: shared decision-making in periviable care; the role of race in end-of-life decision-making, and obstetrical decision-making for periviable delivery management. Her research highlighted substantial gaps in critical deliberative components of shared decision-making—particularly values clarification, preference, and elicitation.
Neonatologists described themselves primarily as informants, rather than partners in the decision- making process, and were reluctant to provide guidance recommendations in response to patient’s requests for advice. This research stemmed, in part, from her concern with the documented disparity in the utilization of hospice. Specifically, blacks and Latinos are more likely to undergo aggressive life-sustaining interventions at the end-of-life.
Tucker-Edmonds research found that neonates born to black and Latina women were more likely to be intubated, but there was no difference in mode of delivery. These descriptive studies generated hypothesis regarding specialty-specific differences in obstetrical and neonatal counseling and decision-making that led to the development of a simulation-based pilot study to test the effect of race and insurer on the content and quality of periviable counseling. In the end, her research revealed that shared decision-making may be utilized differently in counseling black Medicaid-insured patients versus white privately-insured patients.
Finally, with existing research documenting the nature and influence of neonatologists on making management decisions for periviable deliveries, Tucker-Edmonds took the focus back one step to the role of obstetricians who are the first to provide counseling to patients. Developing two nationally-representative surveys of obstetrical generalists and Maternal Fetal Medicine specialist, she documented that obstetricians’ personal characteristics, such as age, gender, and religiosity, as well as their practice characteristics, such as region and teaching-affiliation, are linked to practice patterns.
Selected Publications
Identifying Strategies to Improve Shared Decision Making for Pregnant Patients' Decisions about Prenatal Genetic Screens and Diagnostic Tests
Reducing decisional conflict in decisions about prenatal genetic testing: the impact of a dyadic intervention at the start of prenatal care
Relationship Between Healthcare Team Segregation & Receipt Of Care By A Cardiologist According To Patient Race
Association Between Race, Cardiology Care, and the Receipt of Guideline-Directed Medical Therapy in Peripartum Cardiomyopathy
Mitigating Misogynoir: Inclusive Professionalism as a Health Equity Strategy